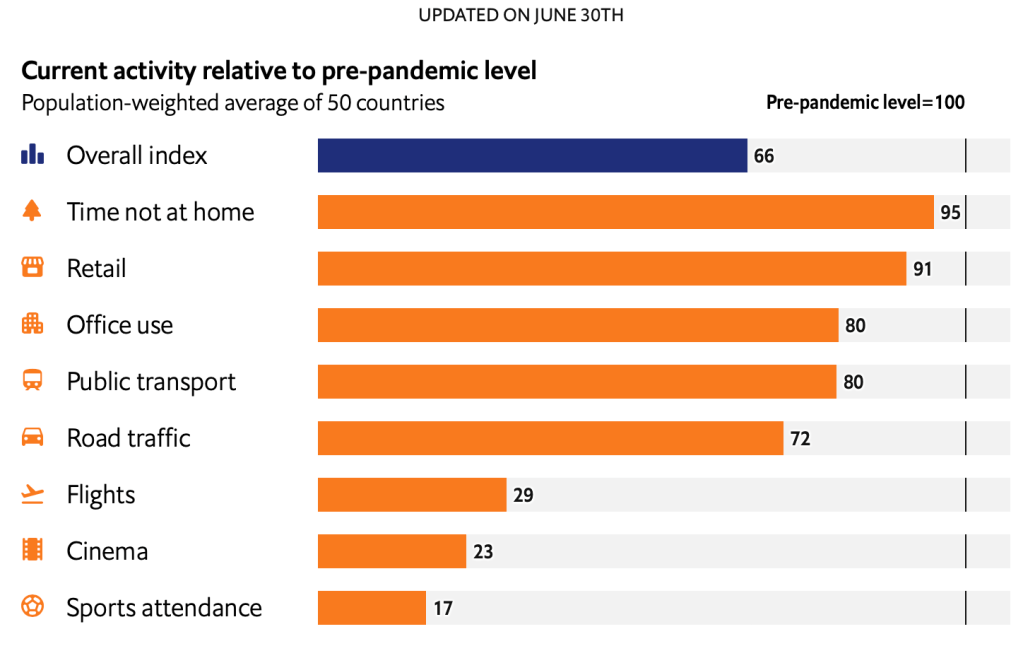
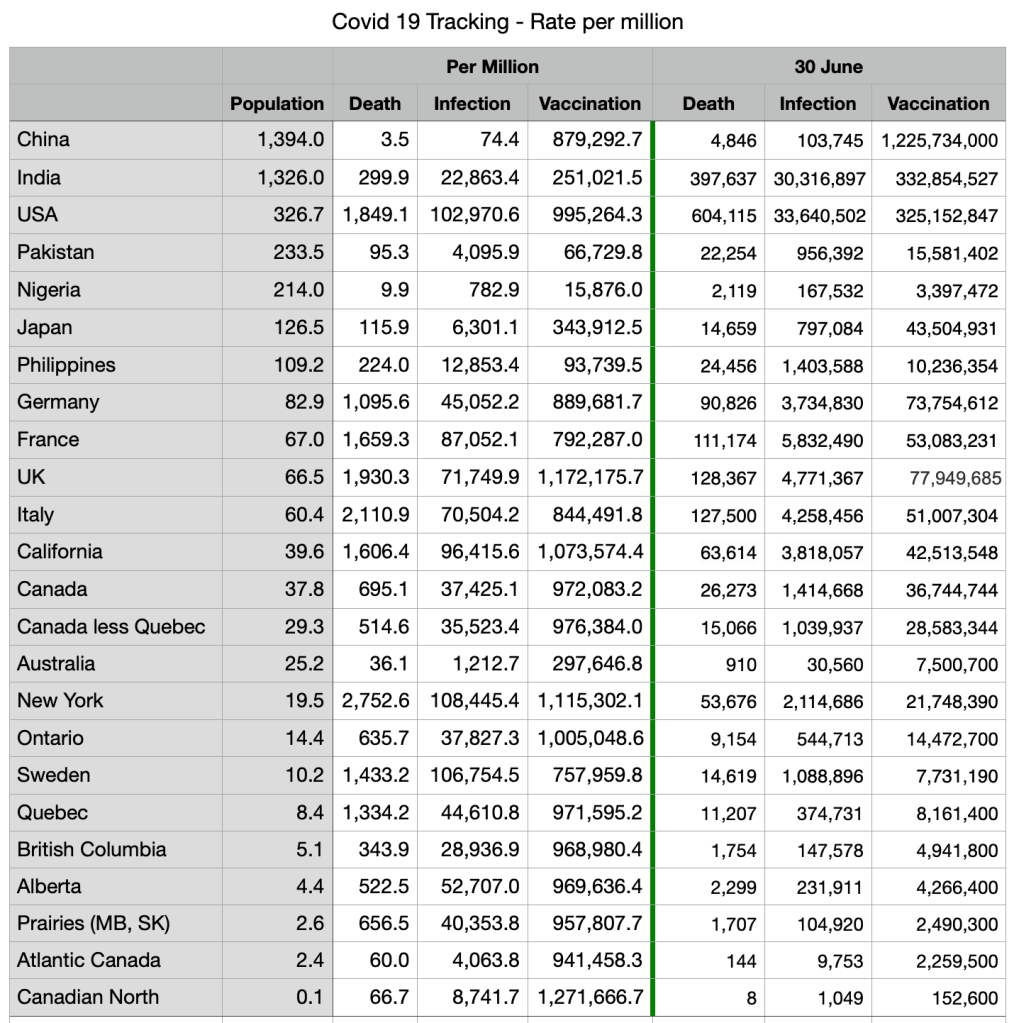
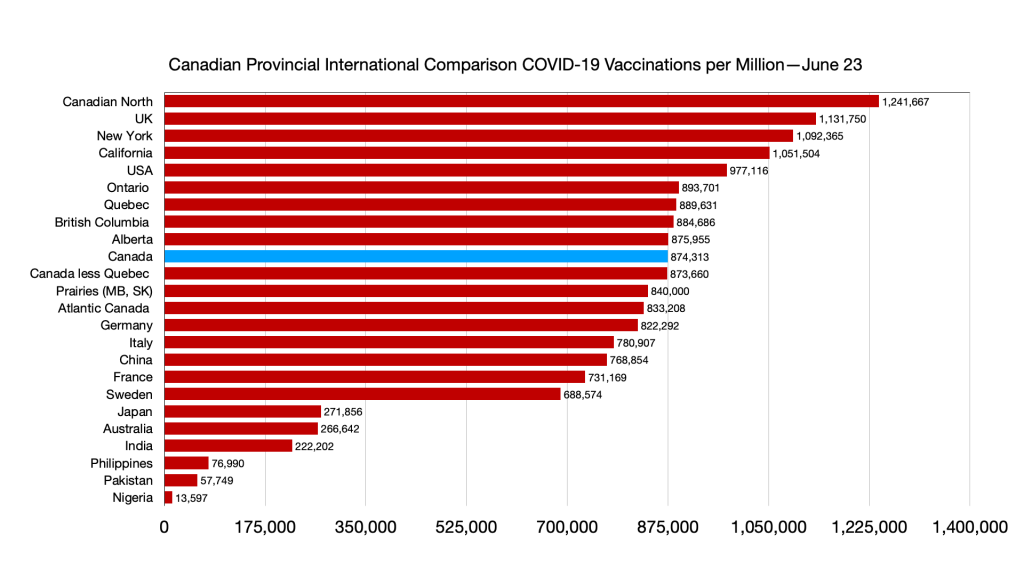
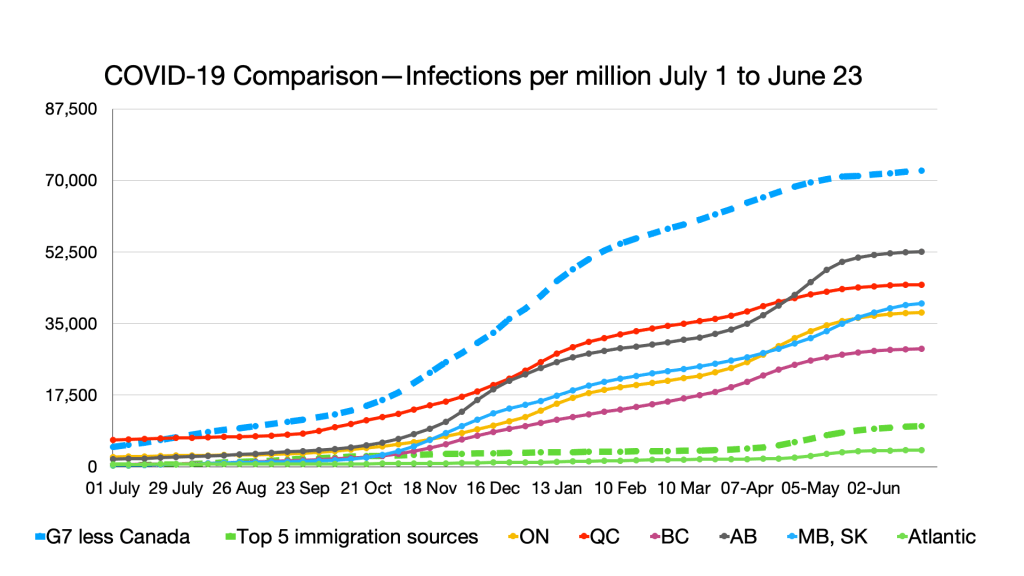
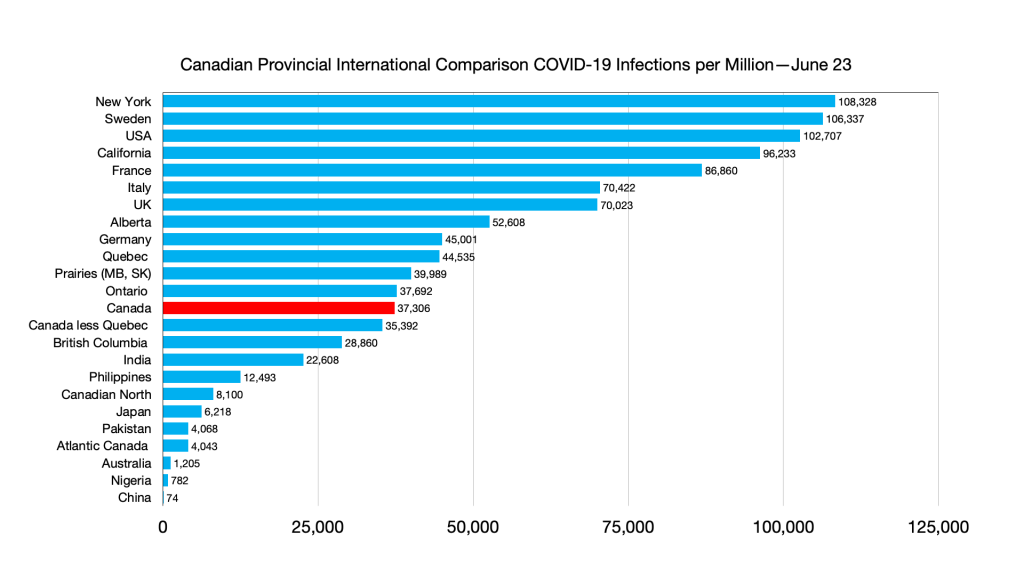
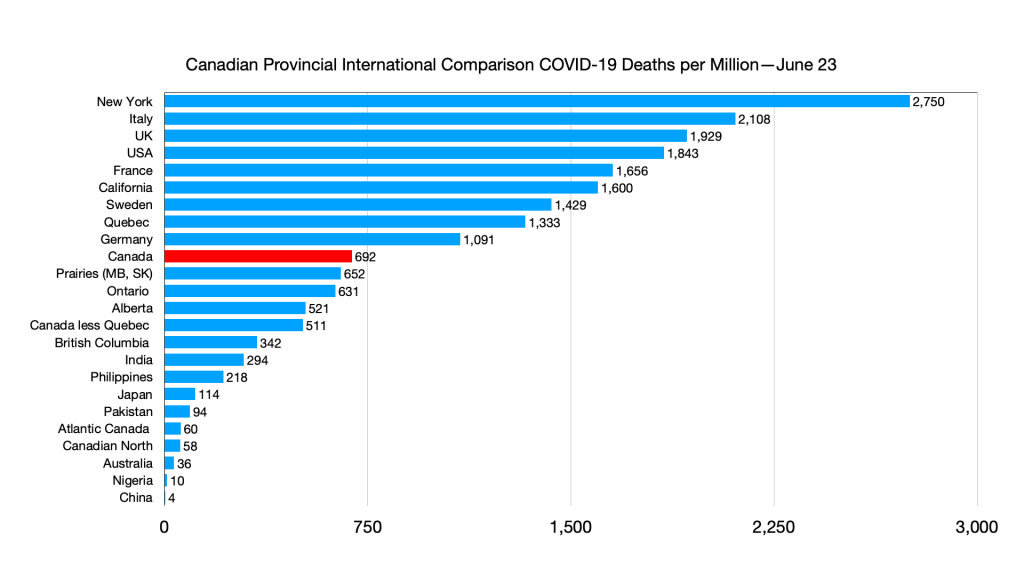
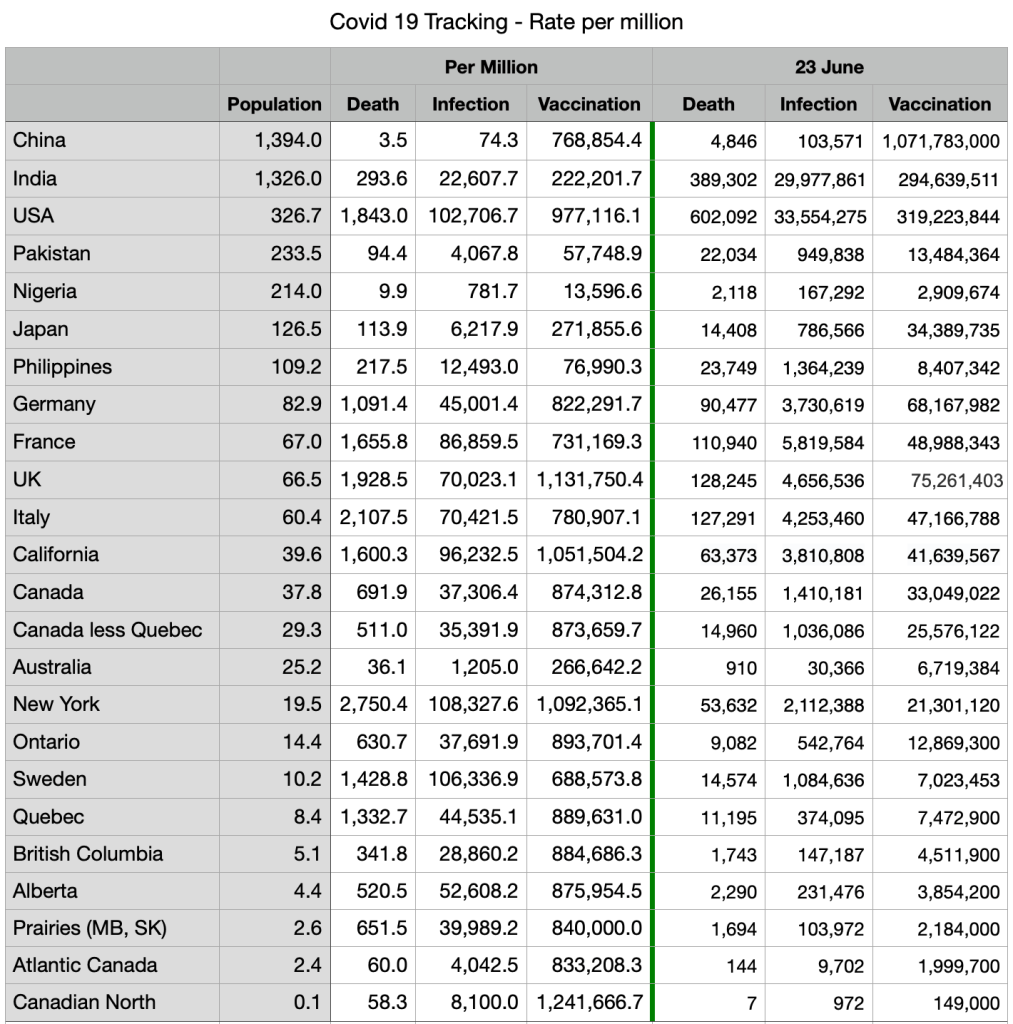
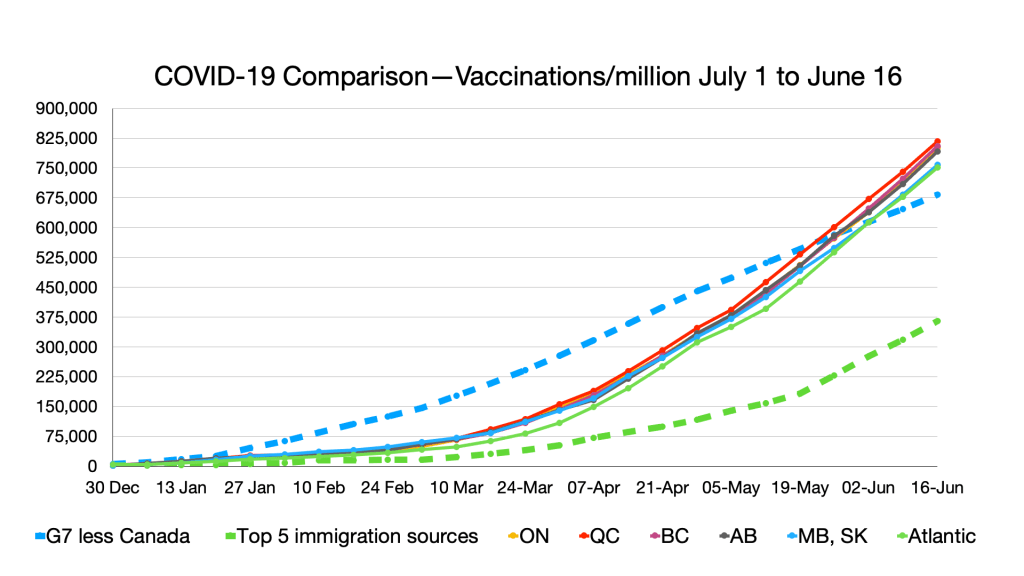
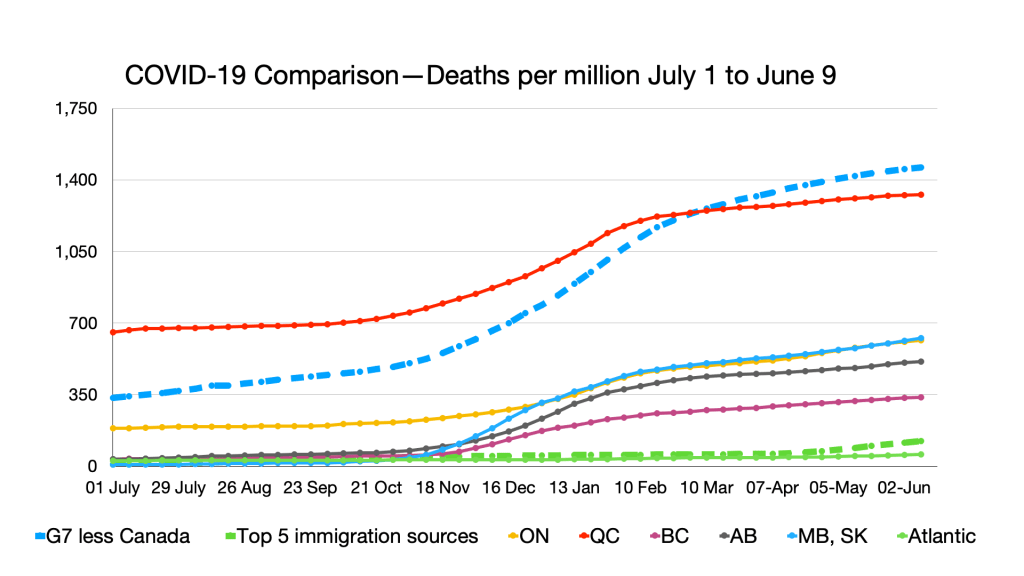
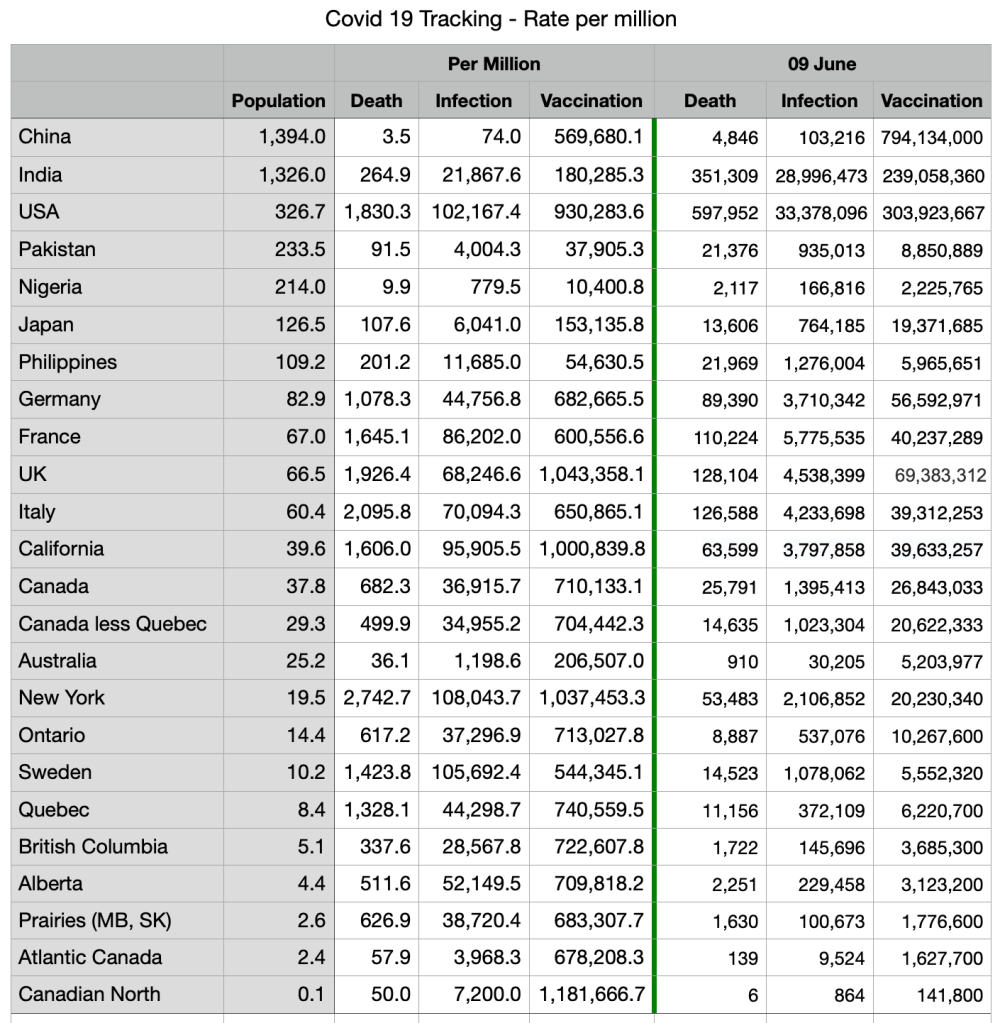
The latest charts, compiled 23 June as overall rates in Canada continue to decline along with increased vaccinations (still largely first dose, fully vaccinated 20.8 percent, most EU countries are between 25 to 35%).
Interesting data on the relative weakness of Chinese vaccines, likely to undermine the Chinese government’s vaccine diplomacy:
Mongolia promised its people a “Covid-free summer.” Bahrain said there would be a “return to normal life.” The tiny island nation of the Seychelles aimed to jump-start its economy.
All three put their faith, at least in part, in easily accessibleChinese-made vaccines, which would allow them to roll out ambitious inoculation programs when much of the world was going without.
But instead of freedom from the coronavirus, all three countries are now battling a surge in infections.
China kicked off its vaccine diplomacy campaign last year by pledging to provide a shot that would be safe and effective at preventing severe cases of Covid-19. Less certain at the time was how successful it and other vaccines would be at curbing transmission.
Now, examples from several countries suggest that the Chinese vaccines may not be very effective at preventing the spread of the virus, particularly the new variants. The experiences of those countries lay bare a harsh reality facing a postpandemic world: The degree of recovery may depend on which vaccines governments give to their people.
In the Seychelles, Chile, Bahrain and Mongolia, 50 to 68 percent of the populations have been fully inoculated, outpacing the United States, according to Our World in Data, a data tracking project. All four ranked among the top 10 countries with the worst Covid outbreaks as recently as last week, according to data from The New York Times. And all four are mostly using shots made by two Chinese vaccine makers, Sinopharm and Sinovac Biotech.
“If the vaccines are sufficiently good, we should not see this pattern,” said Jin Dongyan, a virologist at the University of Hong Kong. “The Chinese have a responsibility to remedy this.”
Scientists don’t know for certain why some countries with relatively high inoculation rates are suffering new outbreaks. Variants, social controls that are eased too quickly and careless behavior after only the first of a two-shot regimen are possibilities. But the breakthrough infections could have lasting consequences.
In the United States, about 45 percent of the population is fully vaccinated, mostly with doses made by Pfizer-BioNTech and Moderna. Cases have dropped 94 percent over six months.
Israel provided shots from Pfizer and has the second-highest vaccination rate in the world, after the Seychelles. The number of new daily confirmed Covid-19 cases per million in Israel is now around 4.95.
In the Seychelles, which relied mostly on Sinopharm, that number is more than 716 cases per million.
Disparities such as these could create a world in which three types of countries emerge from the pandemic — the wealthy nations that used their resources to secure Pfizer-BioNTech and Moderna shots, the poorer countries that are far away from immunizing a majority of citizens, and then those that are fully inoculated but only partly protected.
China, as well as the more than 90 nations that have received the Chinese shots, may end up in the third group, contending with rolling lockdowns, testing and limits on day-to-day life for months or years to come. Economies could remain held back. And as more citizens question the efficacy of Chinese doses, persuading unvaccinated people to line up for shots may also become more difficult.
One month after receiving his second dose of Sinopharm, Otgonjargal Baatar fell ill and tested positive for Covid-19. Mr. Otgonjargal, a 31-year-old miner, spent nine days in a hospital in Ulaanbaatar, the capital of Mongolia. He said he was now questioning the usefulness of the shot.
“People were convinced that if we were vaccinated, the summer will be free of Covid,” he said. “Now it turns out that it’s not true.”
Beijing saw its vaccine diplomacy as an opportunity to emerge from the pandemic as a more influential global power. China’s top leader, Xi Jinping, pledged to deliver a Chinese shot that could be easily stored and transported to millions of people around the world. He called it a “global public good.”
Mongolia was a beneficiary, jumping at the chance to score millions of Sinopharm shots. The small country quickly rolled out an inoculation program and eased restrictions. It has now vaccinated 52 percent of its population. But on Sunday, it recorded 2,400 new infections, a quadrupling from a month before.
In a statement, China’s Foreign Ministry said it did not see a link between the recent outbreaks and its vaccines. It cited the World Health Organization as saying that vaccination rates in certain countries had not reached sufficient levels to prevent outbreaks, and that countries needed to continue to maintain controls.
“Relevant reports and data also show that many countries that use Chinese-made vaccines have expressed that they are safe and reliable, and have played a good role in their epidemic prevention efforts,” the ministry said. China has also emphasized that its vaccines target severe disease rather than transmission.
No vaccine fully prevents transmission, and people can still fall ill after being inoculated, but the relatively low efficacy rates of Chinese shots have been identified as a possible cause of the recent outbreaks.
The Pfizer-BioNTech and Moderna vaccines have efficacy rates of more than 90 percent. A variety of other vaccines — including AstraZeneca and Johnson & Johnson — have efficacy rates of around 70 percent. The Sinopharm vaccine developed with the Beijing Institute of Biological Products has an efficacy rate of 78.1 percent; the Sinovac vaccine has an efficacy rate of 51 percent.
The Chinese companies have not released much clinical data to show how their vaccines work at preventing transmission. On Monday, Shao Yiming, an epidemiologist with the Chinese Center for Disease Control and Prevention, said China needed to fully vaccinate 80 to 85 percent of its population to achieve herd immunity, revising a previous official estimate of 70 percent.
Data on breakthrough infections has not been made available, either, though a Sinovac study out of Chile showed that the vaccine was less effective than those from Pfizer-BioNTech and Moderna at preventing infection among vaccinated individuals.
A representative from Sinopharm hung up the phone when reached for comment. Sinovac did not respond to a request for comment.
William Schaffner, medical director of the National Foundation for Infectious Diseases at Vanderbilt University, said the efficacy rates of Chinese shots could be low enough “to sustain some transmission, as well as create illness of a substantial amount in the highly vaccinated population, even though it keeps people largely out of the hospital.”
Despite the spike in cases, officials in both the Seychelles and Mongolia have defended Sinopharm, saying it is effective in preventing severe cases of the disease.
Batbayar Ochirbat, head researcher of the Scientific Advisory Group for Emergencies at Mongolia’s Ministry of Health, said Mongolia had made the right decision to go with the Chinese-made shot, in part because it had helped keep the mortality rate low in the country. Data from Mongolia showed that the Sinopharm vaccine was actually more protective than the doses developed by AstraZeneca and Sputnik, a Russian vaccine, according to the Health Ministry.
The reason for the surge in Mongolia, Mr. Batbayar said, is that the country reopened too quickly, and many people believed they were protected after only one dose.
“I think you could say Mongolians celebrated too early,” he said. “My advice is the celebrations should start after the full vaccinations, so this is the lesson learned. There was too much confidence.”
Some health officials and scientists are less confident.
Nikolai Petrovsky, a professor at the College of Medicine and Public Health at Flinders University in Australia, said that with all of the evidence, it would be reasonable to assume the Sinopharm vaccine had minimal effect on curbing transmission. A major risk with the Chinese inoculation is that vaccinated people may have few or no symptoms and still spread the virus to others, he said.
“I think that this complexity has been lost on most decision makers around the world.”
In Indonesia, where a new variant is spreading, more than 350 doctors and health care workers recently came down with Covid-19 despite being fully vaccinated with Sinovac, according to the risk mitigation team of the Indonesian Medical Association. Across the country, 61 doctors died between February and June 7. Ten of them had taken the Chinese-made vaccine, the association said.
The numbers were enough to make Kenneth Mak, Singapore’s director of medical services, question the use of Sinovac. “It’s not a problem associated with Pfizer,” Mr. Mak said at a news conferenceon Friday. “This is actually a problem associated with the Sinovac vaccine.”
Bahrain and the United Arab Emirates were the first two countries to approve the Sinopharm shot, even before late-stage clinical trial data was released. Since then, there have been extensive reports of vaccinated people falling ill in both countries. In a statement, the Bahraini government’s media office said the kingdom’s vaccine rollout had been “efficient and successful to date.”
Still, last month officials from Bahrain and the United Arab Emirates announced that they would offer a third booster shot. The choices: Pfizer or more Sinopharm.